Biosimilars
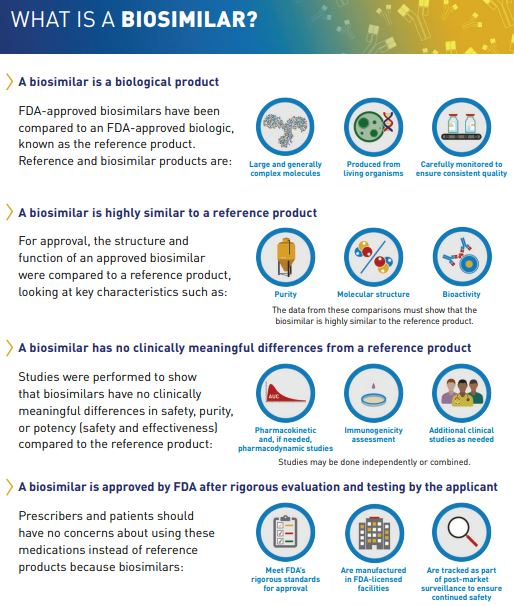
A biosimilar product is a biological product that is “highly similar and has no clinically meaningful differences from an existing FDA-approved reference product."[1] A drug manufacturer developing a proposed biosimilar must demonstrate that its product is “highly similar” to the referenced product by analyzing the structure and function of both the referenced product and the biosimilar. Advanced technology is used to compare product characteristics such as purity, chemical identity, and bioactivity. Minor differences in clinically inactive components within the biosimilar and the reference drug are acceptable. The FDA evaluates any differences between the biosimilar and the reference drug to ensure that approval standards are met.[1]
It is important to note that biosimilars are not the same as generic drugs. Biosimilars and generic drugs are both versions of brand name drugs that may represent more affordable treatment options for patients. Biosimilars and generics are approved through different (abbreviated) pathways, avoiding the need to duplicate clinical trials. The active ingredients in generic drugs are the same as those in brand name drugs. The manufacturer of a generic drug must demonstrate that the generic is a bioequivalent to the brand name drug. In contrast, biosimilar drug manufacturers must demonstrate that the biosimilar is “highly similar” to the reference product, with the exception of minor differences in clinically inactive components. Drug manufacturers must also demonstrate that there are “no clinically meaningful differences between the biosimilar and the reference product in terms of safety and effectiveness.”[1]
The Patient Protection and Affordable Care Act (PPAC Act) (signed into law by President Obama in 2010) amended the Public Health Service Act (PHS Act) to create an abbreviated and more streamlined approval pathway for biosimilars. These new statutory provisions are also referred to as the Biologics Price Competition and Innovation Act of 2009.[2] Biological products, in general, are the fastest-growing class of therapeutic products in the United States, accounting for a significant and increasing percentage of healthcare costs. The abbreviated pathway to approval was established in order to increase access to lifesaving medications and also to lower healthcare costs through increased competition.[3]
BIOSIMILARITY FACTORS
The FDA’s Center for Drug Evaluation and Research and the Center for Biologics Evaluation and Research have outlined several factors that sponsors should consider when assessing a proposed product’s biosimilarity to that of a reference product:
- Expression system: Differences between the chosen expression system and the reference product should be carefully considered as the type of expression system and host cell will considerably affect the types of process-related and product-related substances that may be present.
- Manufacturing process: A complete breakdown of the manufacturing process, which includes characterization, adventitious agent safety, process controls, and specifications for the adequate product review, should be established during product development.
- Assessment of physicochemical properties: All relevant characteristics of the protein product should be considered to maximize the potential for detecting differences in quality attributes.
- Functional activities: Functional assays serve to complement physicochemical analyses and measure the qualitative function of the protein product.
- Receptor binding and immunochemical properties: Analytical tests should be performed to characterize if binding or immunochemical properties are a part of the activity attributed to the protein product.
- Impurities: Applicants should characterize, identify, and quantify impurities that are either product and/or process related as defined in ICH Q6B.
- Reference product and reference standards: Analytical studies should not only focus on the characterization of the potential biosimilar in isolation but should be part of a broad comparison that includes the proposed biosimilar, the reference product, applicable reference standards, and the deliberation of relevant publicly disseminated information.
- Finished drug product: Product characterization studies should be done on the most downstream product best suited for the analytical procedures.
- Stability: Physicochemical and functional comparative studies should be initiated and performed under multiple stress conditions.[4]
BIOSIMILAR APPROVAL PROCESS
All FDA-approved biological products, including biosimilar products, undergo rigorous evaluation to ensure that the drug meets standards for efficacy, safety, and quality. A reference product is approved in a traditional manner—the application must contain all data and information necessary to demonstrate the safety and effectiveness of the drug. This data generally includes clinical trials for the disease indications sought by the manufacturer. The goal of a biosimilar program is not to establish the safety and efficacy of the proposed product, but rather the goal is to demonstrate biosimilarity between the proposed biosimilar and the reference product. The manufacturer of the biosimilar is responsible for demonstrating that the proposed biosimilar is “highly similar” to the FDA reference product. The data is “generated and evaluated in a stepwise fashion that begins with a foundation of detailed analytical (structural and functional) characterization and comparison of the products, moving on to animal studies if necessary and then to comparative clinical studies.”[5] Biosimilar manufacturers often do not need to conduct as many clinical trials, essentially fast-tracking these products to the market. This provides patients with additional therapeutic options at a lower cost. The data required for the approval of a biosimilar product include:
- Analytical studies that demonstrate that the biological product is “highly similar to the reference product,” despite any minor differences in clinically inactive components.
- Animal studies, including an assessment of toxicity.
- At least one clinical study that sufficiently demonstrates safety, purity, and potency of the biosimilar product in one or more of the indications for which the reference product is licensed. This may include assessments of immunogenicity, pharmacokinetics, and sometimes pharmacodynamics. It may also include a comparative clinical study.
- Data demonstrating that the proposed interchangeable product is expected to produce the same clinical result as the reference product.
- Data to demonstrate that—for a product administered multiple times to a patient—switching between the reference product and the proposed interchangeable product does not increase safety risks or decrease effectiveness (in comparison to if one were to use only the reference product).
BIOSIMILAR APPROVAL POINTS OF CONTACT
If one has specific questions pertaining to the development of a biosimilar product not yet submitted in a 351(k) Biologics License Application (marketing application), they can contact the Therapeutic Biologics and Biosimilars Staff at:
ONDTherapeuticBiologicsandBiosimilarsPMStaff@fda.hhs.gov
If one has questions regarding a product development program of 351(k) Biologics License Application (BLA) for which they are the sponsor, applicant, or authorized representative, they are instructed to contact the Regulatory Project Manager in the Office of New Drugs review division that is assigned to their application.[6] Biologics are regulated by the FDA’s Center for Drug Evaluation and Research (CDER). Applications for CDER-regulated drugs are reviewed by a multidisciplinary team. For biologics, the Chemistry, Manufacturing, and Controls (CMC) information is reviewed by personnel in the Office of Biotechnology Products. Manufacturing-related information is reviewed by the Therapeutics Facilities Review Branch in the Office of Compliance.[7]
MORE ON BIOSIMILARS
The following bullets reflect additional information on biosimilars, from the FDA:
- Biosimilar and Interchangeable Products
- Biosimilar Development, Review, and Approval
- Prescribing Biosimilar and Interchangeable Products
- Biosimilar Product Information
- Industry Information and Guidance
- Webinars, Presentations, and Articles
- Health Care Provider Materials
- Patient Materials
Updated by Theresa Pipher, November 2020

Comments are closed.